by Carrie Bauman
Once considered the cornerstone of American healthcare, private practices are only a small segment of today’s healthcare ecosystem. Rising costs, shrinking reimbursements, regulatory pressures, and mounting administrative burdens have already caused many independent physicians to sell to hospitals or private equity groups. In fact, over 74% of physicians were employed by hospitals or corporate entities by 2023, a significant increase from just a few years prior.
This dramatic shift is not just about ownership, it is about autonomy, financial sustainability, and patient care quality. But there is a path forward. With the right mix of AI-powered analytics and operational foresight, private practices can reclaim efficiency, improve margins, and maintain independence.
One of the most cited reasons for practice distress is the shrinking margins from Medicare, Medicaid, and commercial insurance reimbursements. The 2024 CMS Physician Fee Schedule cut reimbursement rates yet again, and inflation-adjusted payments have dropped by over 26% since 2001, according to the AMA. Physicians are doing more — and getting paid less. This is unsustainable for practices already juggling overhead costs like rent, staff salaries, and technology investments.
Private practice physicians report spending up to 50% of their time on non-clinical tasks. Prior authorization, documentation, compliance, and MIPS reporting are administrative burdens that are burning out physicians. According to a 2023 Medscape report, 53% of physicians say too much bureaucracy is the top cause of burnout. Worse, many small practices lack the infrastructure or personnel to manage these complexities effectively.
Skilled billing staff, medical assistants, and front-desk workers are harder to retain. Salary inflation, labor shortages, and post-pandemic workforce shifts have left practices scrambling to keep up. Without qualified teams, billing errors, denied claims, and long wait times become the norm, directly hurting both revenue and patient experience.
The shift to hospital or corporate ownership often provides short-term stability. However, it comes with trade-offs:
Hospital-employed physicians must often meet productivity targets, follow corporate protocols, and sacrifice decision-making freedom.
Hospital systems are largely focused on referrals and procedures. Independent practices often prioritize long-term patient care.
While hospital systems negotiate better payer contracts due to patient volumes, they also retain a significant share of physician-generated revenue.
Private practices that stay independent must therefore find smarter, tech-enabled ways to manage margins and scale operations.
Denied claims are one of the largest hidden drains on private practice revenue.
AI and predictive analytics can reduce denial rates by identifying root causes, flagging risky claims before submission, and automating appeals.
Here is where things get optimistic. Today’s AI-driven platforms are not just for large hospital systems. Scalable tools now exist that make it easier for private practices to:
There is no need to spend time running reports from your electronic health record system, importing them into Excel, and analyzing performance before you act. AI automates all these tasks and makes graphics readily available in multiple formats for reporting. Simply log in, review the status, and take actionable steps to resolve issues. Examples of automatically created dashboards include:
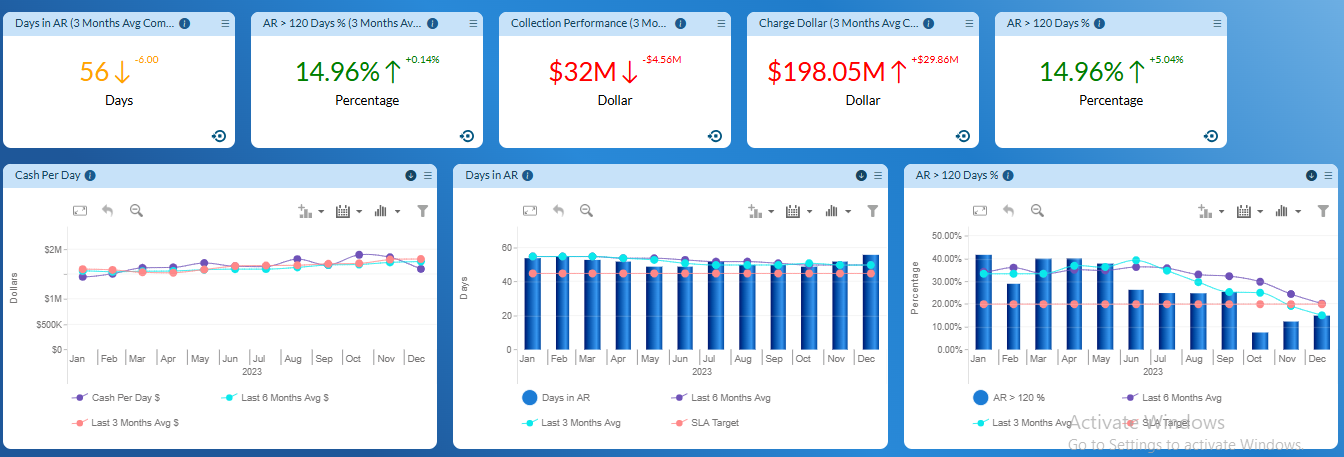
With machine learning capabilities, the system does not just report status, it recommends actions with the highest probability of success. Examples include recommendations on when to follow up, how to rebill, and which payers need intervention.
AI revenue cycle analytics can review millions of claims and flag the ones most likely to be denied even before submission. This pre-billing advice allows your billing team to correct errors, add missing documentation, or proactively initiate peer-to-peer review, improving your first-pass clean claims rate and facilitating higher collections.
Tools like eligibility verification AI and authorization automation solutions use NLP (Natural Language Processing) to extract insurance requirements. They also trigger workflows and reduce staff time by up to 60% for each request.
AI-powered appointment optimization forecasts no-show risks based on patient behavior, weather, and appointment history. Practices using predictive appointment tools report 10–15% fewer no-shows, increasing patient access and optimizing provider schedules.
Using national datasets, some analytics platforms allow practices to compare KPIs like revenue per visit, cost per encounter, or staff-to-provider ratios. These benchmarks provide clarity on where you stand and where to improve.
Today’s private practices require more than excellent clinicians; they need data-driven business leaders. Here is what financial leaders in private practices are focusing on:
These tools do not eliminate the need for regulatory compliance, but they make it more manageable, especially for practices without full-time compliance staff.
If you are in a leadership role at a private practice, here are five immediate steps to future-proof your operations:
Organizations like MGMA and AMA are lobbying for regulatory simplification and better payer transparency. But change is slow. In the meantime, practices that embrace analytics and AI will outperform peers, attract better staff, and retain independence. AI is not about replacing people. It is about augmenting clinical and financial intelligence to thrive in an increasingly complex landscape.
Private practices still matter. They deliver personalized, community-based care and often outperform large systems in patient satisfaction. The pressures they face are real — but so are the solutions. By embracing AI, analytics, and smarter financial operations, private practices can stop reacting to change and start driving it.

A 30-year veteran of healthcare IT, Carrie Bauman is responsible for marketing, communications and business development strategies that drive brand awareness, growth and value for clients, partners and investors.

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431