
by Carrie Bauman
Changing payer and provider requirements pose unique challenges to your organization. There is constant pressure to enhance healthcare operations while maintaining RCM optimization. Artificial Intelligence (AI) is no longer a futuristic concept; it is revolutionizing AI in revenue cycle management by increasing operational efficiency in healthcare and boosting healthcare financial performance. However, AI cannot replace human expertise entirely. Instead, the right balance between AI and your RCM teams is essential to drive operational success.
AI has become a game-changer in healthcare operations. AI enhances revenue cycle workflows by automating claim submissions, enhancing coding accuracy with predictive analytics, streamlining prior authorizations, and improving patient financial engagement through AI-driven chatbots and virtual assistants.
According to a recent survey by Black Book, 68% of healthcare leaders say AI-driven RCM optimization has improved their financial performance.
By integrating AI into your healthcare operations, you can reduce administrative burdens, find areas of revenue leakage and fix them, and enhance the overall patient experience. AI is most effective when it works alongside your RCM teams to improve their productivity and operational performance.
Your RCM team plays a crucial role in ensuring financial stability, but inefficiencies and manual tasks often slow down productivity. AI can empower your staff by:

AI automates repetitive tasks such as eligibility verification, claim scrubbing, and payment posting, allowing your RCM team to focus on higher-value tasks like patient advocacy and financial planning.
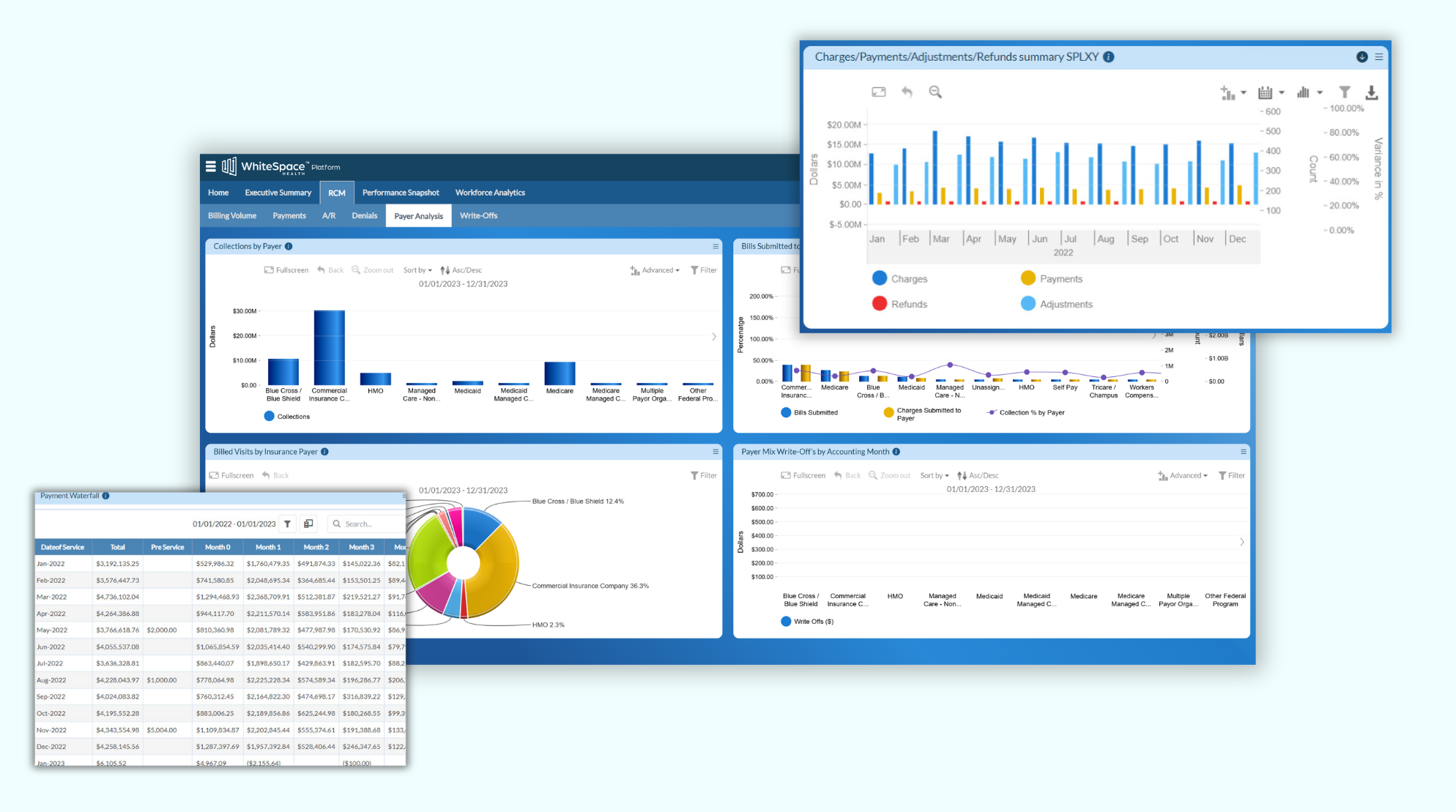
AI-driven analytics platforms, such as WhiteSpace Health, deliver real-time data insights, helping your team identify revenue leakage, track payment trends, and proactively address claim denials.
AI can predict payer behavior and flag high-risk claims, enabling your RCM team to prioritize workload and prevent revenue loss.
AI-driven dashboards track employee productivity, highlight skill gaps, and offer personalized training recommendations to enhance staff performance.
AI chatbots and virtual assistants streamline patient interactions, reducing call center workloads and improving patient satisfaction.
By leveraging AI to manage routine tasks, your RCM professionals can spend more time on strategic activities, increasing their efficiency and job satisfaction.
Optimizing healthcare operations requires a blend of automation and human expertise. AI enhances operational performance by:
To fully harness AI’s potential, healthcare leaders must follow strategic implementation steps:
Evaluate your existing healthcare operations to identify pain points where AI can add the most value. Focus on inefficiencies in claims processing, revenue cycle delays, and administrative bottlenecks.
Select AI-driven platforms that integrate seamlessly with your EHR and billing systems. Solutions like WhiteSpace Health provide AI-powered analytics that align with your organization’s RCM optimization goals.
AI should complement your staff, not replace them. Invest in training programs that teach your team how to use AI tools effectively, interpret AI-generated insights, and apply them to decision-making processes.
Before a full-scale rollout, test AI solutions in a specific area, such as claims processing or denial management. Monitor performance metrics and gather feedback from your team to refine AI integration.
Continuously track AI’s impact on healthcare financial performance using key performance indicators (KPIs). Use real-time analytics to make data-driven adjustments and ensure AI remains aligned with your operational goals.
WhiteSpace Health’s advanced analytics platform empowers your healthcare operations by identifying revenue leakage, enhancing compliance, providing actionable insights, and optimizing workforce efficiency. AI-driven audits reduce compliance risks, and real-time dashboards help your RCM teams make data-driven decisions, ensuring long-term financial success. By integrating AI-driven analytics, your organization can achieve:
AI will continue to reshape RCM optimization, making it more efficient, accurate, and scalable. Future advancements include:
Enhanced forecasting models will allow healthcare organizations to predict revenue trends and adjust financial strategies proactively.
AI will further streamline prior authorization processes, reducing approval times and preventing treatment delays.
More sophisticated virtual assistants will handle patient financial questions, reducing call center workloads and improving patient engagement.
AI will enhance fraud prevention by detecting billing irregularities and preventing financial losses.
AI systems will continuously improve by learning from new billing data and refining their accuracy in claims processing and denials management.
To maximize healthcare financial performance, your organization must strike the right balance between AI-driven automation and human expertise. AI enhances healthcare operations, but your RCM teams’ strategic insights and problem-solving skills remain essential. By leveraging platforms like WhiteSpace Health, you can optimize RCM optimization, improve team productivity, and achieve operational efficiency in healthcare.
AI is not a replacement for human intelligence, it is an enabler. By integrating AI strategically and empowering your RCM team, you can create a highly efficient revenue cycle that supports both financial success and superior patient care.
Are you ready to transform your healthcare operations with AI? Take the next step with WhiteSpace Health’s cutting-edge analytics today!

A 30-year veteran of healthcare IT, Carrie Bauman is responsible for marketing, communications and business development strategies that drive brand awareness, growth and value for clients, partners and investors.

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431