
by Ivan Bradshaw
The role of AI in RevEval is pivotal in identifying patterns, trends, and areas where practices can recover lost revenue. By analyzing 835/837 claim data and a corresponding aged trial balance, AI in the WhiteSpace Health Platform identifies underperforming revenue cycle workstreams. The RevEval Assessment also makes recommendations for resolution of specific claim types and overall improved performance of your revenue cycle. The AI capabilities ensure that the analysis is accurate and insightful, turning large datasets into easily digestible recommendations.
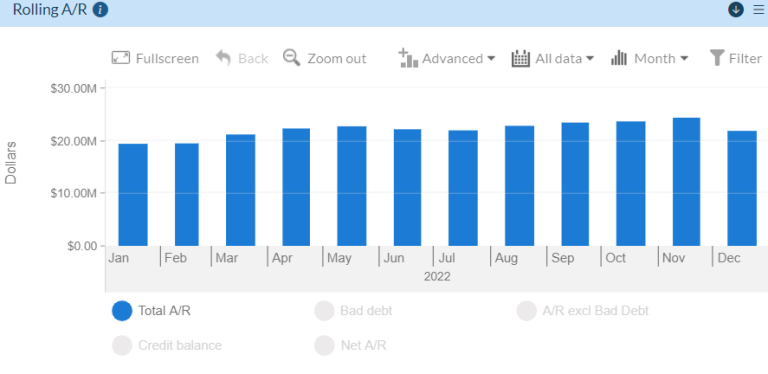
RevEval provides practices with a comprehensive view of their revenue cycle by tracking several key performance indicators (KPIs). These KPIs are categorized into different sections like Accounts Receivable (A/R), Billing Volume, Denials, Patient Responsibility, Payments, Payer Analysis, and Write-offs and Adjustments. Let’s break them down:

The automated data processing within RevEval helps in analyzing billing volume and submission lags, ensuring efficiency in billing practices.
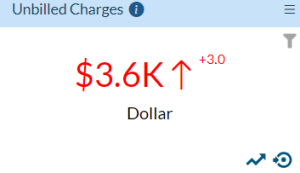
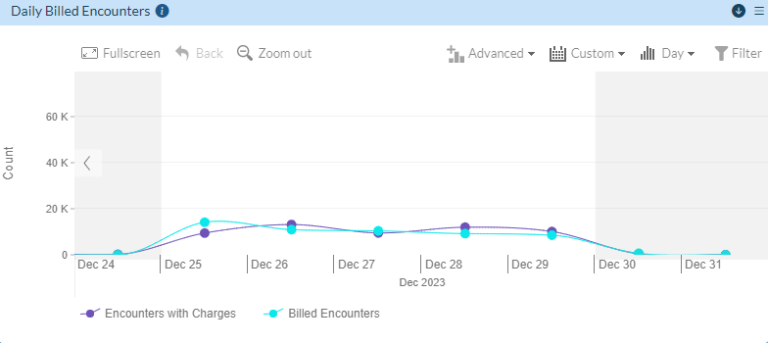
This data-driven approach helps practices reduce lag times and improve overall claim submission efficiency, thereby accelerating cash flow.
Denials are a critical metric for any healthcare provider, and machine learning in data analysis can predict trends, allowing practices to address them proactively.
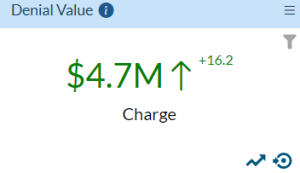
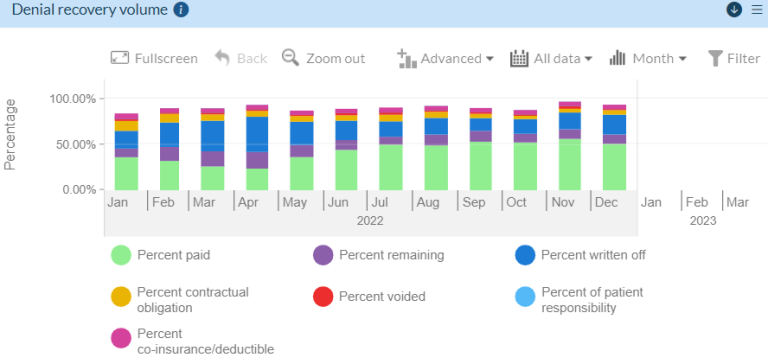
With data-driven insights, RevEval helps reduce denial rates and recover lost revenue faster.
Patient balances can significantly impact revenue collection if not managed effectively. AI in historical data analysis helps practices stay on top of patient A/R metrics.
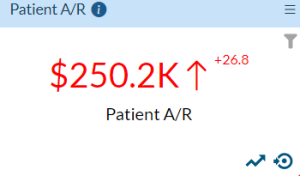
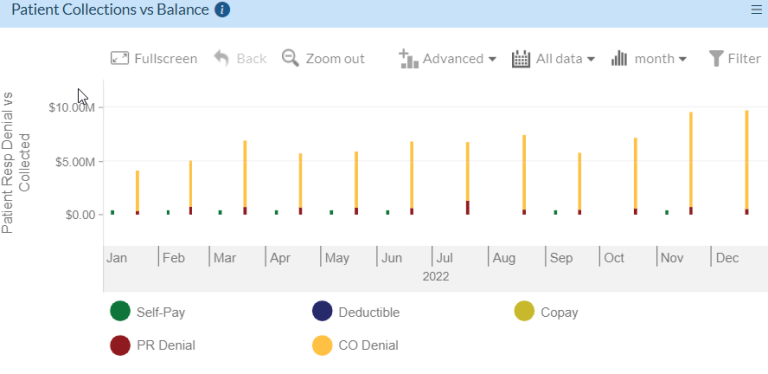
This enables practices to ensure they are collecting patient payments in a timely fashion, reducing overall A/R days.
The payment metrics available through RevEval offer deep data-driven insights into a practice’s cash flow. The healthcare analytics platform uses automated data processing to track payment lags and resolution rates.
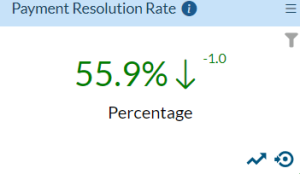
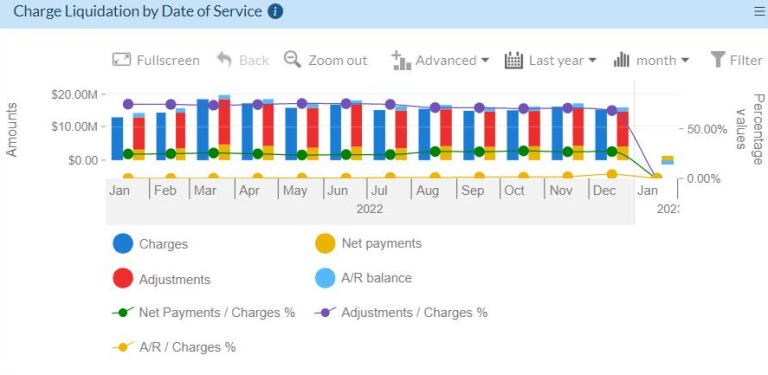
This allows practices to identify payment trends and improve cash collections.
A RevEval Assessment offers a breakdown of payer-specific metrics, helping practices to evaluate payer performance more effectively.
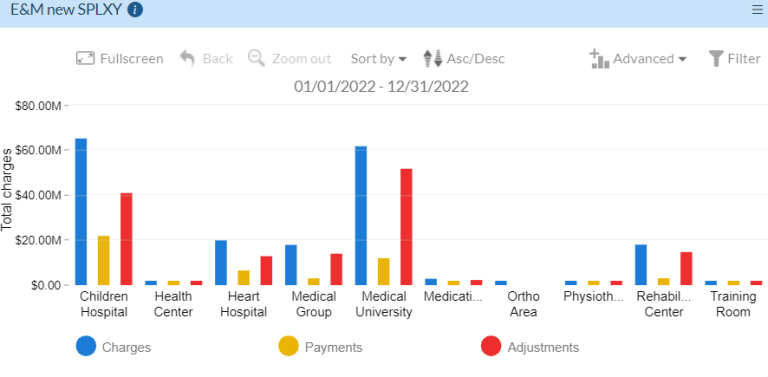
By understanding which payers are performing well, practices can prioritize payer relations and billing strategies accordingly.
Write-offs are an inevitable part of healthcare billing. However, machine learning in data analysis can help minimize unnecessary write-offs and ensure practices are maximizing revenue.
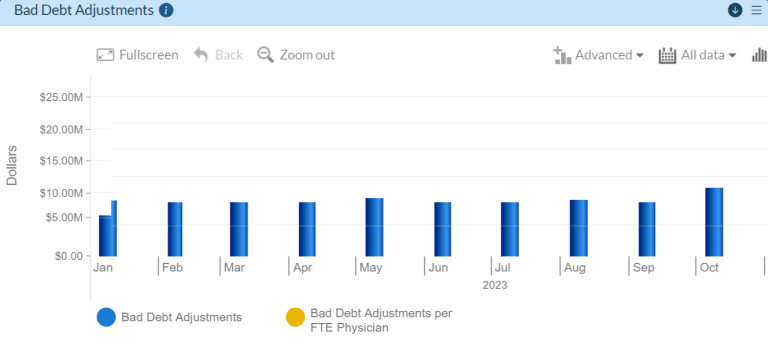
By utilizing AI in historical data analysis, RevEval provides data-driven insights into write-offs and adjustments, helping practices prevent revenue loss.
A RevEval Assessment is a transformative tool for healthcare practices, that uses AI applied to historical data to deliver actionable insights that drive financial improvement. Analytics ensure that practices are not just reviewing historical data, but they are able to actively use it to improve their performance. By offering a comprehensive analysis of KPIs across A/R, billing, denials, payments, and patient responsibility, RevEval delivers data-driven insights that can reshape the financial health of any practice.
As the healthcare industry continues to evolve, adopting AI-powered assessments like RevEval will become essential for practices looking to stay competitive and financially healthy.

Ivan Bradshaw is the vice president of product management at WhiteSpace Health. As a revenue cycle management executive with over 20 years of experience, Ivan is adept at building high-performance teams and creating RCM solutions that stop revenue leakage, improve operational efficiency, and grow top line performance.

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431