by Carrie Bauman
Private payers have found ways to increase their profits by refusing or delaying legitimate medical claims. As a healthcare organization, you may have noticed how these strategies affect your cash flow, disrupt patient care, and escalate administrative burdens. In this blog, we’ll explore how insurance claim delays, denied medical claims and insurance reimbursement delays are common tactics used by private insurers to boost their profits. Additionally, we’ll dive into how effective claims management in healthcare can help mitigate these denials, and the powerful role the WhiteSpace Health platform plays in fighting back against these tactics.

It’s not just your organization’s bottom line that’s affected by these delays and denials. Patients, too, suffer from delayed care, increased costs, and greater health risks.
According to surveys, nearly 14% of all claims were past due for remittance, meaning providers often waited up to six months after delivering services before receiving payment. These delays compromise patient care, as hospitals are forced to keep patients longer than necessary due to insurance companies delaying discharges to post-acute care settings. This can lead to higher rates of secondary infections and other complications.
When you’re left waiting on payments for months, your financial stability is jeopardized. Hospitals with fewer days of cash on hand are unable to reinvest in patient care or meet other obligations. In contrast, major insurers like United Health Group and Cigna have seen their cash on hand increase significantly in recent years. While you struggle with insurance claim delays, insurers are profiting off these tactics, which undermines the entire healthcare ecosystem.
So, how can you combat these aggressive payer tactics? The key is to take a proactive approach to claims management in healthcare, starting with real-time monitoring of your claims and denials.
Using the WhiteSpace Health Analytics Platform, you can better manage and mitigate denied claims by leveraging advanced AI and analytics. Here’s how:
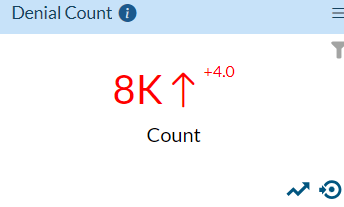
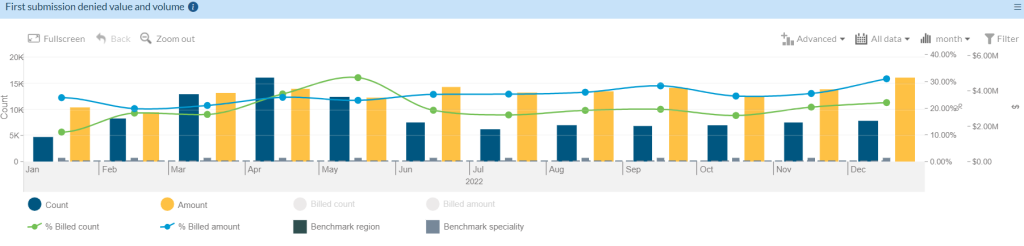
WhiteSpace Health’s platform provides full visibility into denied claims and their financial impact on your organization. By utilizing KPI Smart Cards, you can immediately see which claims need attention, prioritize them, and act fast.
The platform’s AI algorithms identify common denial reasons and provide guidance on how to appeal and recover denied claims. This saves your team significant time by streamlining the insurance claim appeals process.
The highest-performing healthcare organizations consistently recover their most expensive denials first. With WhiteSpace Health, your team can sort claims by value and focus on high-priority denials that can still be overturned.
WhiteSpace Health also allows you to benchmark your denials performance against industry peers, providing insights into how you can improve your processes and become a top performer in claims management in healthcare.
Denials have a far-reaching impact on healthcare organizations, both in terms of direct costs and the hidden costs that often go unnoticed. Here are some key statistics that highlight the financial burden denials place on your practice:
These staggering figures emphasize the need for better tools and processes to manage denials. By using the WhiteSpace Health platform, you can stay ahead of these denials, reduce the costs associated with appeals, and increase your revenue.
You might wonder, what separates the top 25% of healthcare organizations from the rest when it comes to denial management? It comes down to a few key practices, all of which are supported by the WhiteSpace Health platform.
Ensuring that claims are accurately coded is critical to avoiding denials. The WhiteSpace Health platform uses AI to flag coding errors and missing documentation before claims are submitted.
Top organizations resolve their denials quickly. By grouping similar denial types and using smart analytics, WhiteSpace Health streamlines the entire medical claim adjudication process.
Denials management is an ongoing battle, but with the right tools, you can level the playing field. WhiteSpace Health’s AI algorithms analyze historical data to provide clear, actionable steps for your team. Even new employees can quickly learn how to handle denials, recover lost revenue, and ensure that insurance reimbursement delays are minimized.
By implementing the WhiteSpace Health platform, you empower your team with the tools they need to turn denied claims into revenue, reduce administrative costs, and improve your financial stability.
Insurance claim delays and denied medical claims will continue to be a significant challenge for healthcare organizations like yours, but they don’t have to cripple your revenue cycle. By leveraging AI, real-time analytics, and benchmarking tools through the WhiteSpace Health platform, you can stay ahead of the game. Recover more payments, reduce costly appeals, and manage your claims management in healthcare more effectively.
WhiteSpace Health equips your organization to become a top performer, helping you overcome the challenges of insurance claim appeals and avoid insurance reimbursement delays. Get paid what you’re owed faster, improve patient care, and maintain your organization’s financial health by using a denial management system that works for you.


2424 North Federal Highway, Suite 205
Boca Raton, FL 33431