
by Ivan Bradshaw
Missing or invalid information denials occur due to various reasons, such as incomplete patient or provider details, incorrect coding, lack of authorization, missing documentation, duplicate claims, COB issues, or billing inaccuracies. These errors often result from insufficient data, coding errors, knowledge gaps, or procedural misunderstandings.
This type of denial is almost always preventable. By proactively enhancing documentation practices, your organization can ensure the precision needed for submitting claims with “clean” patient and provider details. Strengthening prior authorization protocols and leveraging advanced technology to scrutinize claims for errors before submission also help curb this error type.
It is easy to recommend improving documentation and prior authorization workstreams. The reality is that these processes can be complex, time-consuming and if there is any personal multi-tasking or interruptions while they are in flight, errors and data omissions can occur quite easily.
AI for claim denials has your back. It analyzes your claims to identify missing or invalid information. AI can also perform real-time checks and provide decision support. All three of these automated functions help ensure the accuracy and completeness of the information in claims submissions. Here are specific examples of how AI for claim denials can help catch missing and invalid data errors before claims are released and denials are returned. You may already be using some of them.

AI for claim denials can be used to play an even more key role in reducing missing and invalid information denials. Here are some more sophisticated use cases of AI to reduce this denial type even further.
ML models can be trained to recognize patterns in claims data that are indicative of missing or invalid information. For example, patterns of incomplete or inconsistent data entries can be detected using Classification or Clustering algorithms.
These models assess the quality of data submitted with claims by analyzing various data attributes such as completeness, consistency, accuracy, and timeliness. They can flag missing or invalid information that may lead to claim denials in medical billing.
Using ML-based models (Random Forest) to analyze historical data to identify patterns and trends associated with missing information denials in healthcare, enabling providers to anticipate potential issues and take proactive measures to ensure complete and accurate documentation.
Using an AI model to prevent denials in healthcare from missing or invalid information in medical billing by involving steps such as defining objectives, collecting, and preprocessing data, selecting, and training the model, and integrating it into the workflow.
Using ML models as support tools for claim resolution by considering the patterns and probabilities, the model can provide recommendations to revenue cycle staff. It can suggest the most appropriate actions to take for a specific denied claim, increasing the likelihood of successful resolution, optimizing the efficiency of the revenue cycle, and lowering denial resolution expenses.
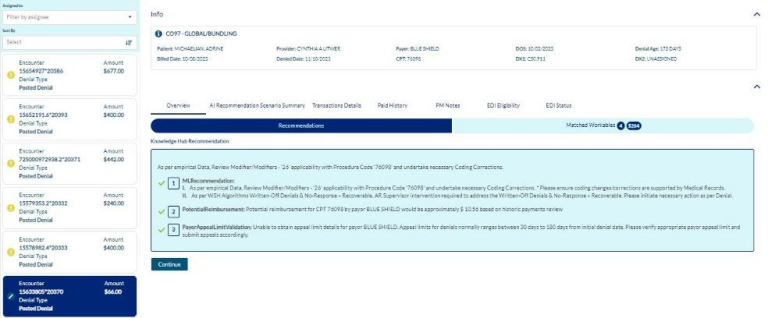
The WhiteSpace Health Platform interprets historical data using AI algorithms and provides recommendations based on successful claims resolutions from the past to create guided steps that staff can quickly read and action. By taking the recommended steps, your organization’s denials have the best chance of being adjudicated and paid. Here is how our AI resolves missing and invalid information denials.
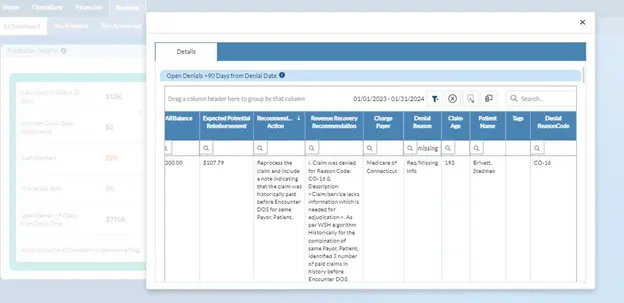
The first step is to locate all the claims that were denied due to missing or invalid information. AI does this for you – and it ensures the accounts are still recoverable before grouping them together.
Step 2
For each claim, the platform delivers guided steps on how to best resolve the denial. These recommendations are based on historical claims evidence of where your organization got paid.
The revenue cycle is largely comprised of codified data in uniform formats. This makes the revenue cycle an excellent starting point for deploying AI to realize greater efficiency of staff and gains in cash collections. When AI algorithms are trained and fine-tuned to traverse ever-growing data sets, their recommendations become even more precise over time, which improves the first-pass clean claims rate and gets you paid faster.
About Ivan Bradshaw

Ivan Bradshaw is the vice president of product management at WhiteSpace Health. As a revenue cycle management executive with over 20 years of experience, Ivan is adept at building high-performance teams and creating RCM solutions that stop revenue leakage, improve
operational efficiency, and grow top-line performance.
Ivan.Bradshaw@whitespacehealth.com

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431