
by Carrie Bauman
Back-offices are increasingly harnessing the power of Artificial Intelligence (AI). These technologies are not merely buzzwords. They introduce essential changes that fundamentally enhance Revenue Cycle Management (RCM), practice management automation, and medical billing automation. Let’s dive deep into the transformative effects of revenue cycle AI on back-office billing operations, providing data-driven healthcare solutions that streamline processes and boost efficiency.
The integration of AI within Revenue Cycle Management processes is revolutionizing the dynamics of healthcare billing. These advanced technologies automate repetitive tasks and analyze vast amounts of data to improve financial outcomes and operational efficiencies. By automating complex processes, AI allows billing staff to focus on more strategic tasks that require human intervention, thus optimizing the overall workflow and reducing errors.
AI offers a plethora of benefits to back-office billing companies such as streamlining operations and enhancing the accuracy of financial transactions. Here’s how these technologies are supporting the front-office with data from patient access operations to make a significant impact

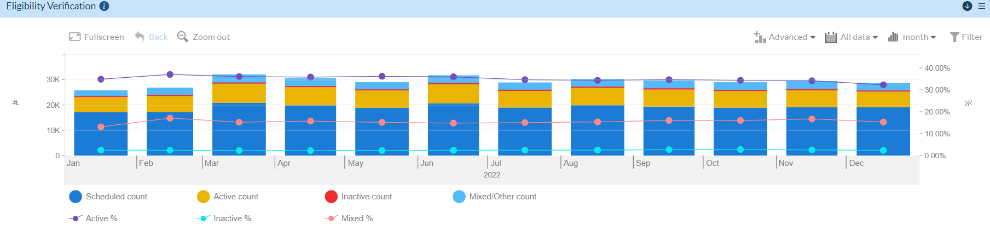
AI platforms quickly verify eligibility, enhancing patient satisfaction and reducing claim denials. They automate the verification process, pulling data from multiple sources to ensure accuracy and completeness.
By predicting patient payment behaviors, AI platforms improve copay collections, thereby increasing revenue upfront. This predictive capability allows practices to tailor their financial conversations with patients, based on likely payment behaviors.
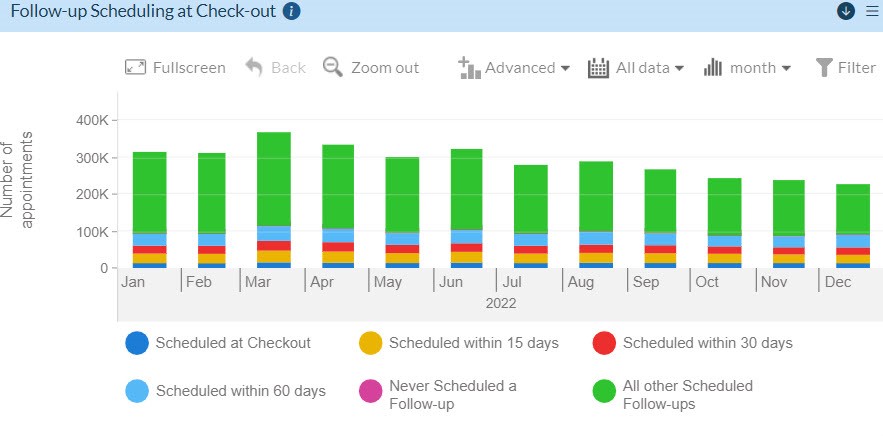
AI-driven scheduling platforms ensure timely follow-ups, enhancing patient care continuity. They can predict the optimal times for follow-ups and streamline appointment scheduling, reducing no-show rates
AI platforms provide detailed insights into patient financial responsibilities and collection rates. They analyze trends over time to identify areas where collections can be improved.
Helps in efficiently tracking and managing prior authorizations to expedite service delivery. AI systems streamline prior authorization by detecting cases that require prior authorization and initiating requests.
By predicting denial risk factors, AI systems inform staff which accounts to double check and verify the specific reasons the claim may be denied prior to releasing to the payer. By ensuring the claim meets specific payer requirements, the likelihood of errors leading to denials is reduced and claims have a higher probability of being paid timely, creating a predictable revenue cycle.
AI powerfully impacts the optimization of billing and charge capture:
Ensures that all services rendered are captured and billed accurately. AI platforms monitor patient encounters in real time to guarantee no billable service goes unbilled.

Tracks the efficiency and timeliness of the billing process. AI systems can flag delays in submission and provide alerts to prevent revenue loss.

Helps in forecasting revenue by analyzing data trends. AI platforms provide predictive analytics to forecast future billing, based on historical data.

AI identifies delays in the billing process, providing actionable insights into areas needing improvement.

AI platforms systematically highlight unbilled services, capturing all potential revenue and minimizing leakage.
Machine Learning identifies and mitigates patterns leading to denials:
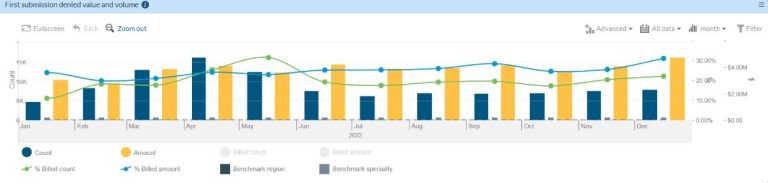
Segregate Denials Value and Volume
Helps prioritize which denials to address based on their financial impact, enabling more strategic denial management.

Identify Denial Recovery Volume
Tracks the volume of successfully overturned denials, providing insights into the effectiveness of denial management strategies.
Know the First Submission Claim Denial Volume
By reducing rework and identifying issues in initial submissions, ML reduces the time and resources spent on reprocessing claims.
Effective management of accounts receivable (A/R) is crucial for maintaining healthy cash flow and ensuring the financial stability of healthcare practices. By leveraging AI, back-office billing companies can transform their approach to monitoring and managing A/R, thereby preventing revenue leaks that can negatively impact a practice’s financial health.

This metric provides a continuous snapshot of outstanding patient balances and insurance reimbursements.

This is a critical measure of the average number of days it takes for a practice to collect payments.

AI can disaggregate A/R data to provide detailed insights on receivables, excluding accounts classified as bad debts.

AI-enhanced platforms analyze the age of accounts receivable to pinpoint how long bills have been outstanding.

AI platforms can maintain and analyze data based on the original financial classifications assigned to different accounts.
AI platforms can analyze the overall percentage of write-offs in relation to the total billing amount, giving a clearer picture of how much revenue is being lost to write-offs.
Double adjustments occur when a bill is adjusted more than once, often due to errors in processing or miscommunication.
AI systems provide a comprehensive analysis of payer trends, which is essential for streamlined billing and negotiation:

One of the most critical aspects of payer trend analysis is identifying discrepancies between the amount billed and the amount paid.
These insights assist in negotiating better rates and understanding payer behaviors, ultimately leading to improved reimbursement.
To fully benefit from AI, back-offices should integrate these technologies with their existing systems, train staff on their benefits, and continuously monitor and adjust algorithms to suit the changing healthcare landscape.
The integration of AI into back-office operations signifies a significant advancement in Automated Medical Billing and AI in RCM Processes. By adopting these technologies, back offices can not only improve accuracy and efficiency but also enhance their overall financial performance. According to MGMA statistics, practices that have embraced these technologies have seen a reduction in denials by up to 20% and an improvement in cash flow by approximately 30%. The future of healthcare billing lies in the effective use of AI, making them not just beneficial but essential for modern revenue cycle management.
About Carrie Bauman

A 30-year veteran in healthcare IT, Carrie Bauman is responsible for marketing, communications and business development strategies that drive brand awareness, growth and value for clients, partners, and investors.
carrie.bauman@whitespacehealth.com

2424 North Federal Highway, Suite 205
Boca Raton, FL 33431