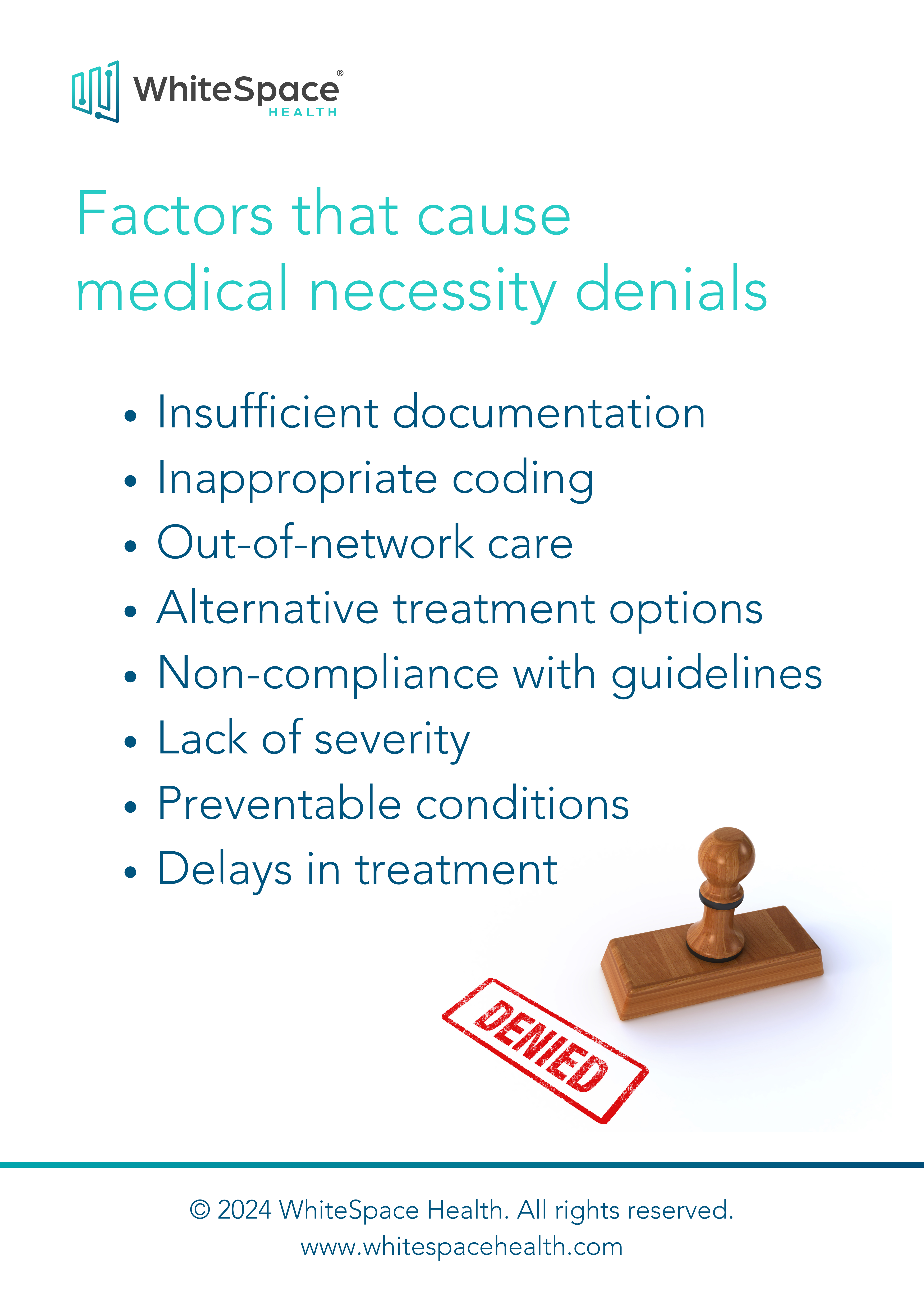
Factors that cause medical necessity denials
Introduction
Medical necessity denials can create significant setbacks for healthcare providers. This infographic outlines key factors that contribute to these denials, including insufficient documentation, inappropriate coding, out-of-network care, and alternative treatment options. Identifying these issues can help healthcare organizations reduce denials and improve the claims approval process.
Conclusion
By addressing the primary causes of medical necessity denials, such as non-compliance with guidelines or preventable conditions, with Platforms like WhiteSpace Health, healthcare providers can improve claim acceptance rates. Proactive measures like better documentation and compliance can streamline operations, minimize denials, and ensure timely reimbursement for necessary treatments.
Let's start the conversation.
+1 888 794.2266